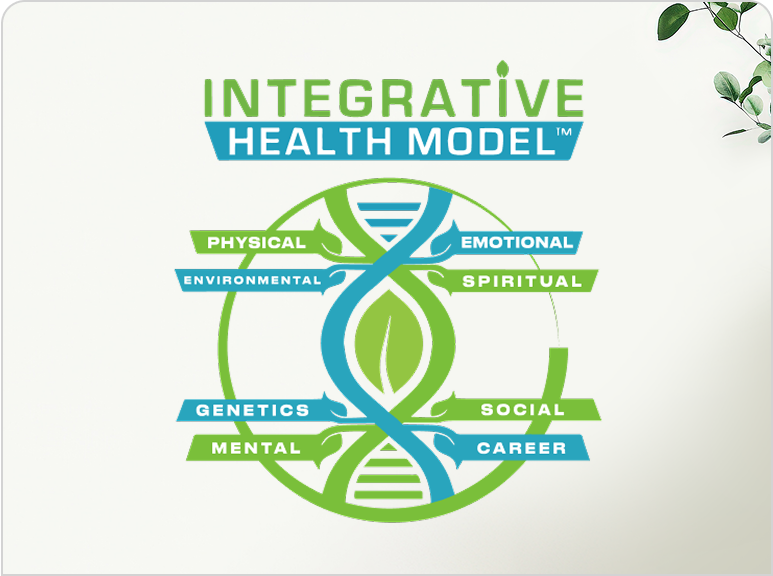
The Whole Person Approach to Recovery

The whole-person approach to recovery treats your mind, body, and spirit together instead of only fixing one problem. This method helps you heal completely by looking at everything in your life that affects your health and happiness.
Think of your health like a puzzle. If you only fix one piece, the whole picture stays broken. The whole-person approach puts all the pieces together. It finds what caused your problems and helps you build a better, healthier life.
What Is the Whole-Person Approach to Recovery?
Understanding the Basics
The whole-person approach looks at every part of you. It treats your body, mind, emotions, and spirit as one connected system. When one part hurts, it affects everything else.
This method is different from regular treatment. Regular treatment might give you medicine and send you home. Whole-person care digs deeper. It asks why you got sick in the first place. According to research from the Substance Abuse and Mental Health Services Administration (SAMHSA), about 21.5 million adults in the United States have both mental health and substance use problems at the same time. These people need care that treats both issues together, not separately.
The Three Main Parts
Mind: Your thoughts, feelings, and mental health need attention. You learn new ways to handle stress and problems. Therapy helps you understand what led to your struggles. You build skills to face life's challenges without falling back into old patterns.
Body: Your physical health gets help too. This means eating better foods, moving your body, and fixing health problems that substances may have caused. Your body needs time to heal and get strong again.
Spirit: This doesn't have to be about religion. It means finding purpose and peace. You might try meditation, yoga, or other practices that help you feel connected and calm. Many people find this gives them hope and strength.
You can't just fix one area and expect to stay healthy. They all work together. If your body feels terrible, your mood drops. If your mind is stressed, your body gets sick. If you feel lost and without purpose, both your body and mind suffer. A 2024 report from the Recovery Research Institute found that 29.3 million U.S. adults have resolved a significant substance use problem. Many found success through approaches that addressed all areas of their lives.
The Science Behind Whole-Person Recovery
How Your Brain and Body Connect
Your brain controls everything in your body. When you struggle with addiction or mental health problems, certain brain areas change. These changes affect how you think, feel, and act.
Research shows that the circuits in your brain that handle rewards, decisions, and emotions can be disrupted by addictive substances. These same brain areas are also affected by depression and anxiety. That's why treating just one issue often doesn't work. The National Institute on Drug Abuse explains that 40-60% of vulnerability to substance use problems comes from genetics. But genes aren't the whole story. Your environment, experiences, and choices matter too.
Co-Occurring Disorders Are Common
Many people have more than one health problem at once. More than one in four adults with serious mental health problems also has a substance use problem. About 55.8% of people with substance use disorders also have a mental illness. These numbers show that treating only one problem leaves the other untreated. The whole-person approach treats both at the same time, which research shows leads to better results.
Evidence That It Works
Studies prove that whole-person care gets better results than single-focus treatment. A SAMHSA review found that programs addressing physical and mental health together significantly reduce substance use and improve overall well-being.
People in whole-person programs report higher satisfaction, feel more empowered, and have better quality of life. Research on relapse rates shows promising trends. While early recovery has relapse rates of 40-60%, after five years of continuous recovery, the relapse rate drops to approximately 15%. Whole-person approaches that build skills and support in all life areas contribute to these improved long-term outcomes.
Key Components of Whole-Person Recovery
Medical and Physical Care
Your body needs help to heal from substance use or mental health struggles. This starts with safe detoxification when needed. Medical professionals monitor you to keep you safe during withdrawal. Physical wellness continues beyond detox with regular check-ups, treatment for medical conditions, help managing chronic pain, nutrition education, and exercise plans that fit your fitness level.
Many people dealing with addiction also have dental problems, sleep issues, or other physical conditions. The whole-person approach addresses all of these, often connecting you with specialists who can help.
Mental Health Support
Your mental health is just as important as your physical health. Therapy helps you understand yourself better and build new skills.
Cognitive Behavioral Therapy (CBT) helps you change negative thought patterns. You learn to catch unhelpful thoughts and replace them with better ones. CBT also teaches coping skills for dealing with cravings and triggers. Trauma-informed care creates a safe space for people who have experienced painful events. It helps you process difficult experiences without overwhelming you.
Group therapy connects you with others who understand your struggles. You learn from their experiences and build supportive relationships. Individual counseling gives you personalized attention for specific issues and goals.
Emotional Wellness
Emotions drive many behaviors. Learning to handle your feelings in healthy ways is crucial for recovery. You'll learn to identify what you're feeling. Many people have numbed their emotions for so long that they don't recognize them anymore. Once you can name your feelings, you can deal with them appropriately.
Emotion regulation skills help you calm down when upset. You learn techniques like deep breathing, mindfulness, and grounding exercises. These tools help you ride out difficult emotions without using substances. Building emotional resilience takes practice, but over time, you get stronger and more confident in handling life's ups and downs.
Spiritual and Purpose-Driven Care
Finding meaning and purpose gives you reasons to stay in recovery. Mindfulness practices help you stay present. Meditation teaches you to observe your thoughts without judgment. Yoga combines physical movement with mental focus. It reduces stress and improves flexibility.
Finding your purpose might mean discovering new interests, reconnecting with old passions, or helping others. Many people in recovery find that giving back to their community brings deep satisfaction and keeps them motivated.
Addressing Root Causes, Not Just Symptoms
Why Symptoms Return
Treating only symptoms is like putting a Band-Aid on a deep wound. It might help for a little while, but the problem comes back. The whole-person approach looks deeper. It asks important questions: What pain are you trying to escape? What needs aren't being met? What life situations push you toward unhealthy coping?
Common Root Causes
Past trauma like childhood abuse, neglect, or other traumatic experiences often lie at the heart of substance use problems. Trauma changes how your brain works and can leave you feeling unsafe, anxious, or disconnected.
Untreated mental health conditions frequently co-occur with addiction. Depression, anxiety, PTSD, and other conditions need proper treatment. Sometimes the mental health problem came first and people used substances to self-medicate. Chronic stress from work, relationships, finances, or health problems wears you down. Environmental medicine approaches recognize how external factors affect your health.
Social isolation hurts recovery. Humans need connection. Loneliness and lack of support make recovery much harder. Sometimes addiction runs in families. You might have grown up watching family members use substances to cope.
Healing the Root Causes
Trauma therapy helps you process painful experiences safely. Techniques like EMDR (Eye Movement Desensitization and Reprocessing) can reduce the emotional charge of traumatic memories. Treating co-occurring mental health conditions often includes both therapy and medication when needed. Integrated mental health support addresses these conditions alongside addiction.
Building new coping skills gives you alternatives to substance use. You learn healthy ways to manage stress, process emotions, and solve problems. Creating a support network might mean rebuilding damaged relationships or forming new connections through support groups and sober social activities.
Creating Your Personal Recovery Plan

Assessment and Evaluation
Every person's recovery journey is different. A good whole-person recovery plan starts with understanding your specific needs. Comprehensive assessment looks at your substance use history, mental health symptoms, physical health conditions, family relationships, work situation, housing stability, strengths you already have, and goals for your recovery.
This assessment isn't about judgment. It's about gathering information to create the best plan for you. Be honest with your treatment team.
Setting Realistic Goals
Goals give you direction and motivation. Short-term goals might include completing detox safely, attending therapy regularly, and learning new coping skills. Long-term goals might look like staying sober for a year or more, returning to work or school, repairing relationships, and developing hobbies.
Your goals should be specific, measurable, and achievable. "Feel better" is too vague. "Attend three support group meetings each week" is clear and concrete.
Choosing Your Treatment Team
Whole-person recovery often involves multiple professionals working together. Your team might include a primary care doctor, psychiatrist, therapist, substance abuse counselor, nutritionist, and peer support specialist. Naturopathic medicine approaches can complement traditional treatment by addressing health from a natural, whole-body perspective.
All these professionals should communicate with each other. Integrated care means everyone knows what everyone else is doing.
Building Your Daily Routine
Structure helps in recovery. Start your day with practices that set a positive tone like meditation, exercise, a healthy breakfast, or journaling. Throughout the day, balance work or responsibilities with self-care. Wind down in the evening with relaxing activities and get enough sleep.
Consistency matters more than perfection. If you miss part of your routine one day, just get back to it the next day.
The Role of Nutrition and Exercise
How Food Affects Recovery
Your brain and body need proper fuel to heal. Good nutrition stabilizes mood and energy levels, reduces cravings for substances, supports brain healing, strengthens your immune system, and improves sleep quality.
Focus on whole foods like fruits, vegetables, lean proteins, whole grains, and healthy fats. Stay hydrated by drinking plenty of water. Limit sugar and caffeine, as they can cause mood swings and sleep problems. Nutrition and weight management services can provide personalized guidance.
Benefits of Physical Activity
Exercise is powerful medicine for both body and mind. Physical activity reduces stress and anxiety naturally, improves mood by releasing feel-good chemicals, helps you sleep better, builds confidence, and creates opportunities for social connection.
Start small if you're not used to exercising. A 10-minute walk counts. Find activities you enjoy like swimming, dancing, hiking, or team sports. When exercise feels fun, you're more likely to stick with it.
Sleep and Recovery
Quality sleep is essential for healing. Poor sleep makes everything harder. When you're tired, you're more likely to feel depressed, anxious, or irritable. Cravings feel stronger and making good decisions becomes harder.
Go to bed and wake up at the same times every day. Create a dark, quiet, cool sleeping environment. Avoid screens for an hour before bed. If sleep problems persist, sleep disorders treatment can address underlying issues.
Social Support and Relationships
Why Connection Matters
Humans need healthy relationships to thrive. Isolation makes recovery nearly impossible. Research consistently shows that strong social support improves recovery outcomes. People with supportive relationships are more likely to stay sober, feel happier, and handle stress better.
But not all relationships are helpful. Part of whole-person recovery involves evaluating your relationships and making tough choices about who deserves space in your life.
Rebuilding Family Relationships
Addiction damages families. Trust breaks and communication fails. Healing these relationships takes time and effort from everyone involved. Family therapy helps everyone understand addiction as an illness. You learn to communicate better and set healthy boundaries.
Making amends means taking responsibility for harm you caused. Trust rebuilds slowly through consistent actions, not words. Some family relationships might not be repairable right away, and that's okay.
Building New Supportive Friendships
You might need to let go of friendships that revolved around substance use. Good places to meet supportive people include support group meetings, recovery community centers, volunteer organizations, classes or hobby groups, and recovery-focused social events.
These friendships often feel more authentic. When you connect with people who know and support the real you, it feels different.
Support Groups and Peer Support
Support groups connect you with others walking a similar path. 12-Step Programs like Alcoholics Anonymous (AA) and Narcotics Anonymous (NA) emphasize acceptance, spiritual growth, and helping others. SMART Recovery offers an alternative that focuses on self-empowerment and scientific research.
Try different groups to find what fits you best. Peer support specialists are people in recovery who have received training to help others. They understand your struggles from personal experience.
Healthy Boundaries
Setting boundaries protects your recovery. Boundaries define what you will and won't accept from others. You might need boundaries around who you spend time with, where you go, and when you need time alone.
Learning to say no takes practice. Many people in recovery have spent years being people-pleasers. Setting boundaries feels uncomfortable at first but gets easier with time.
Addressing Co-Occurring Disorders

Understanding Dual Diagnosis
Many people have both substance use disorders and mental health conditions. Common mental health conditions that occur with addiction include depression, anxiety disorders, PTSD, bipolar disorder, and ADHD.
These conditions interact in complex ways. Sometimes the mental health condition came first, and substance use was an attempt to self-medicate. Other times, substance use triggered or worsened mental health symptoms.
Why Integrated Treatment Is Essential
Treating only the addiction while ignoring mental health problems doesn't work. The untreated mental health condition will likely trigger relapse. Integrated treatment addresses both conditions simultaneously.
According to SAMHSA research, integrated treatment leads to better symptom reduction for both conditions, lower relapse rates, improved quality of life, and better overall health outcomes.
Medication-Assisted Treatment
For some people, medications play an important role in recovery. For opioid use disorder, medications like methadone, buprenorphine, and naltrexone reduce cravings and withdrawal symptoms. Research shows these medications cut the risk of death by half.
For alcohol use disorder, medications help reduce drinking or maintain abstinence. For mental health conditions, antidepressants, mood stabilizers, and other psychiatric medications can help manage symptoms.
Medication isn't "cheating" or a sign of weakness. It's a tool, just like therapy or support groups. Holistic medicine approaches can complement medication with natural therapies.
Trauma-Informed Care in Recovery
Many people with addiction have experienced trauma. Trauma changes how your brain works and can leave you feeling constantly on edge, emotionally numb, unable to trust others, or depressed.
Trauma-informed care creates safety first. Therapists help you process experiences at a pace that feels manageable. Techniques include EMDR, Cognitive Processing Therapy, and mindfulness practices. As you process trauma, many symptoms of addiction and mental health problems often improve naturally.
Life Skills and Practical Support
Developing Coping Skills
Healthy coping skills replace old, harmful patterns. For stress, try deep breathing exercises, taking a walk, talking to a trusted friend, or engaging in a hobby. For cravings, use the HALT method (Am I Hungry, Angry, Lonely, or Tired?), call your sponsor, or attend a support group meeting.
Build a toolkit of many strategies. Then you'll always have options when challenges arise.
Financial Management and Employment
Money problems create stress that can threaten recovery. Create a realistic budget, address debts one at a time, and avoid impulsive spending. Many people need help finding or returning to work. Vocational rehabilitation programs help you identify skills, create a resume, practice interview skills, and connect with employers who support recovery.
Housing and Stability
Stable housing is crucial for recovery. Sober living homes provide a structured, substance-free environment. You live with others in recovery, follow house rules, and receive support. If you have your own housing, make it recovery-friendly by removing all substances and creating a calm, organized space.
Transportation and Access to Care
Getting to appointments, work, and support groups matters. Solutions include public transportation passes, recovery program transportation services, carpooling, and telehealth appointments. Telemedicine services make it easier to access care from home.
Measuring Progress and Adjusting Your Plan
What Success Looks Like
Recovery isn't all-or-nothing. Signs of progress might include days or months of sobriety, improved relationships, better physical health, reduced mental health symptoms, stable housing and employment, and feeling hope about the future.
Success doesn't mean perfection. You'll have good days and hard days. Progress isn't always linear. What matters is the overall direction you're moving.
Tracking Your Recovery
Keeping track of progress helps you see how far you've come. Journal about your thoughts and feelings. Use a sobriety app to count days. Complete regular self-assessments with your therapist. Celebrate milestones, no matter how small.
Looking back at where you started shows real progress, even when current challenges feel overwhelming.
When to Adjust Your Treatment Plan
Your needs change as you progress in recovery. Signs you might need to adjust your plan include struggling with cravings more than usual, mental health symptoms getting worse, isolating yourself from support, or current treatments not feeling helpful.
Talk openly with your treatment team about what's working and what isn't. Good providers welcome this feedback and will work with you to adjust your plan.
Preventing Relapse
Understanding Relapse
Relapse means returning to substance use after a period of abstinence. Studies show 40-60% of people relapse in the first year. However, relapse doesn't have to be part of your story. Many people achieve long-term recovery without relapse.
Warning Signs of Relapse
Relapse usually happens in stages. Emotional relapse comes first. You might stop going to support groups, isolate yourself, or stop taking care of yourself. Mental relapse comes next. Part of you wants to stay sober, but another part starts thinking about using. Physical relapse is when you actually use substances again.
Recognizing early warning signs gives you time to get help before physical relapse happens.
Your Relapse Prevention Plan
A written relapse prevention plan should include your specific triggers, warning signs that you're struggling, coping strategies for each trigger, contact information for your support team, and steps to take if you feel close to using.
Identify your triggers. Common triggers include stress at work or home, certain social situations, specific locations, conflict in relationships, or boredom and loneliness. For each trigger, have a specific response ready. Build multiple layers of support.
If Relapse Happens
If you use substances again, don't give up. Stop using immediately and get to a safe place. Reach out for help right away. Be honest with your treatment team about what happened. Identify what led to the relapse and adjust your recovery plan.
Many people say relapse taught them important lessons. They strengthened their recovery by learning from the experience.
The Ongoing Journey of Recovery
Recovery Is a Lifestyle, Not a Destination
Recovery isn't something you finish. It's an ongoing process of growth and healing. Even after years of sobriety, you continue learning and developing. Most people find that viewing recovery as a lifestyle brings freedom. You don't have to be perfect. You're always growing.
Continuing Care and Aftercare
After completing intensive treatment, continuing care helps you maintain progress. This might include weekly therapy sessions, regular support group meetings, and wellness activities. The amount of support you need decreases over time for most people, but staying connected to recovery support helps maintain your gains.
Growth and Self-Discovery
Many people discover that recovery opens doors they never imagined. Without substances clouding your life, you have energy and clarity to pursue education, develop new hobbies, travel, deepen relationships, and give back to your community. Recovery reveals your true self and many people find talents and strengths they didn't know they had.
Helping Others
After establishing your own recovery, helping others who struggle can be deeply rewarding. This might mean sponsoring someone in a 12-step program, volunteering at a recovery center, or sharing your story to inspire others. Helping others reinforces your own recovery and gives it deeper meaning.
Resources and Getting Started
Finding Whole-Person Treatment Programs
When searching for help, look for programs that treat co-occurring mental health and substance use disorders, offer multiple types of therapy, include medical care and medication management, provide nutritional support and wellness activities, and create individualized treatment plans.
Online and Community Resources
SAMHSA National Helpline at 1-800-662-HELP (4357) provides free, confidential, 24/7 treatment referral. Alcoholics Anonymous (AA) has meetings in virtually every community. Narcotics Anonymous (NA) focuses on drug addiction. SMART Recovery offers a science-based alternative. The 988 Suicide & Crisis Lifeline is available when you call or text 988.
Insurance and Payment Options
Cost shouldn't prevent you from getting help. Most insurance plans cover substance use and mental health treatment. Medicaid and Medicare provide coverage. Treatment programs offer sliding scale fees based on income. Don't let money concerns stop you from seeking help.
Taking the First Step
Starting can feel overwhelming. You don't have to have everything figured out. Just take one small step. That first step might be calling a helpline, attending one support group meeting, telling someone you trust that you need help, or scheduling an appointment with a doctor.
Each small action builds momentum. Before you know it, you're on your path to healing.
Final Thoughts
The whole-person approach to recovery offers hope for lasting healing. By addressing your mind, body, and spirit together, you create a strong foundation for a healthy, fulfilling life.
Recovery is possible. Millions of people have walked this path before you. They've rebuilt their lives, repaired relationships, and discovered joy they never thought possible. You can too.
Remember to treat all aspects of yourself, not just symptoms. Address root causes, not just surface problems. Build a strong support system. Use multiple tools and strategies. Be patient with yourself. Celebrate progress, no matter how small. Recovery is a journey, not a destination.
You deserve a life free from the pain of addiction and mental health struggles. You deserve to thrive, not just survive. The whole-person approach gives you the tools, support, and framework to build that life. Your recovery matters. Your life matters. Take that first step today. Better days are ahead.
You May Also Like
.png)
.png)



%201.png)


.png)
.png)



.png)
.png)
.png)
.png)
.png)
.png)
.png)
.png)

.png)
.png)
.png)
.png)

.png)
.png)

.png)
.png)






.png)




.png)
.png)
.png)

.png)

.png)