Can I Manage My Thyroid Without Medication?

No, you generally cannot manage your thyroid without medication if you have a diagnosed thyroid disorder. While diet, stress control, and supplements can support thyroid health, they cannot replace the hormones your body fails to produce. Medical treatment is usually necessary to keep thyroid levels stable and prevent serious complications.
What Is Hypothyroidism And Why Does It Occur?
Hypothyroidism means the thyroid gland produces insufficient hormones. The thyroid, a small butterfly-shaped gland in the neck, makes hormones T3 and T4. These hormones control metabolism, body temperature, heart rate, energy levels, and cognitive function.
Low thyroid hormone causes fatigue, weight gain, cold sensitivity, brain fog, dry skin, hair loss, depression, and constipation. Research shows 11.7% of Americans had hypothyroidism in 2019, up from 9.5% in 2012. Women face higher risk than men. People over 60 show the highest prevalence rates.
Hashimoto's disease ranks as the most common cause in America. This autoimmune condition makes the immune system attack thyroid tissue. Iodine deficiency causes hypothyroidism in some countries but remains rare in America. Thyroid surgery, radioactive iodine treatment, certain medications, and pituitary problems also trigger hypothyroidism.
When Does Hypothyroidism Require Medication?
Medication becomes mandatory after thyroid removal, radioactive iodine treatment, or severe hormone deficiency. The body cannot function without adequate thyroid hormones. No diet, supplement, or lifestyle change can replace these essential hormones when the thyroid cannot produce them.
Complete thyroid removal leaves the body unable to produce hormones. After total thyroidectomy, patients need daily thyroid hormone replacement permanently. Radioactive iodine treatment destroys thyroid cells gradually. The damaged cells cannot regenerate. Patients eventually develop hypothyroidism requiring medication.
Hashimoto's disease typically requires lifelong medication. This autoimmune condition progressively damages the thyroid. Over time, the gland loses its ability to produce sufficient hormones. Early intervention with naturopathic medicine may slow progression in some cases.
Overt hypothyroidism always requires treatment. This diagnosis appears when TSH exceeds 10 mIU/L and T4 drops below normal range. The body cannot compensate for such severe hormone deficiency. Medication restores normal function quickly and safely.
What Do Blood Test Numbers Mean For Thyroid Health?

TSH above 4.0 signals possible thyroid dysfunction while TSH above 10 requires immediate medication. TSH measures thyroid-stimulating hormone from the pituitary gland. High TSH means the pituitary sends stronger signals to boost thyroid hormone production. Normal TSH ranges from 0.5 to 4.0 mIU/L in most labs.
TSH between 5 and 10 with normal T4 indicates subclinical hypothyroidism. This mild form may not cause obvious symptoms. Doctors debate whether to treat this range. The decision depends on symptoms, antibody status, age, and other factors.
TSH above 10 requires treatment regardless of symptoms. Research shows patients with TSH above 10 face significantly higher cardiovascular risks and metabolic complications. Treatment prevents long-term damage to the heart, brain, and other organs.
Free T4 measures inactive thyroid hormone circulating in blood. Low Free T4 with high TSH confirms overt hypothyroidism. Free T3 measures active thyroid hormone that cells actually use. Some people convert T4 to T3 poorly. They may have normal TSH and T4 but low T3. This causes persistent symptoms despite normal lab results.
Can Subclinical Hypothyroidism Reverse Without Medication?
About one-third of people with subclinical hypothyroidism see normal levels return without treatment. A Greek study examined 291 patients with uncertain initial diagnoses. After 6-8 weeks off medication, 61% maintained normal thyroid function without medication.
Several factors predict successful medication discontinuation. Normal thyroid ultrasound suggests minimal structural damage. Negative thyroid antibodies indicate no autoimmune attack. TSH below 8 at initial diagnosis improves reversal odds. Younger age at diagnosis also helps.
The American Thyroid Association notes one-third of subclinical hypothyroidism cases resolve spontaneously within three months. The thyroid recovers on its own in these situations. However, two-thirds of cases require treatment. Regular monitoring determines which patients improve and which need medication.
What Foods Support Thyroid Function?
Iodine, selenium, iron, and vitamin D support thyroid hormone production. Adults need 150 micrograms of iodine daily. Iodized salt provides this amount easily. Fish, shellfish, dairy products, and eggs also contribute iodine.
Selenium helps convert T4 into active T3. Just two Brazil nuts daily supply adequate selenium. Tuna, halibut, turkey, chicken, eggs, and whole grain bread also supply selenium. Research showed selenium supplementation reduced thyroid antibodies in Hashimoto's patients. Those interested in autoimmune disorder management should discuss selenium levels with their healthcare provider.
Iron supports thyroid hormone synthesis. Lean red meat provides highly absorbable heme iron. Spinach, fortified cereals, beans, and lentils supply non-heme iron. Vitamin D deficiency links strongly to autoimmune thyroid disease. Sun exposure for 15-20 minutes daily produces adequate vitamin D in most people.
Soy contains isoflavones that may interfere with thyroid hormone production. People taking levothyroxine should avoid soy products for at least four hours after medication. Cruciferous vegetables contain goitrogens but cooking significantly reduces goitrogen content. Normal cooked servings pose no risk.
Sugar and processed foods increase systemic inflammation. Inflammation slows the conversion of T4 to active T3. Reducing refined sugars, white flour products, and artificial ingredients decreases inflammatory burden.
Should People With Hypothyroidism Avoid Gluten?
People with celiac disease or gluten sensitivity who have hypothyroidism benefit from gluten-free diets. No evidence supports gluten avoidance for all hypothyroid patients.
Celiac disease and Hashimoto's thyroiditis frequently occur together. Research demonstrates gluten-free diets improve thyroid function in patients with both conditions. Some patients reduced or eliminated thyroid medication needs after one year gluten-free.
However, most hypothyroid patients without celiac disease do not benefit from gluten elimination. Testing for celiac disease makes sense before eliminating gluten. Blood tests detect celiac antibodies. These tests only work while consuming gluten.
What Supplements Help Thyroid Function?
Vitamin B-12, probiotics, and selenium supplements may support thyroid health alongside medication. Supplements cannot replace thyroid hormone medication in overt hypothyroidism.
Hypothyroidism depletes vitamin B-12 levels. Supplementing B-12 may reduce fatigue and improve energy in deficient patients. Food sources include eggs, meat, poultry, fish, and dairy products. Doses of 500-1000 micrograms daily help most deficient people.
A 2020 clinical trial examined 60 hypothyroid patients taking levothyroxine. Half received synbiotic supplementation combining prebiotics and probiotics. After eight weeks, the synbiotic group showed significantly decreased TSH levels and lower levothyroxine dose requirements. Those exploring digestive health optimization may find probiotics particularly helpful.
Ashwagandha may help regulate thyroid hormones in subclinical hypothyroidism. Turmeric reduces inflammation throughout the body. However, kelp and high-dose iodine supplements pose significant risks. Excess iodine can trigger or worsen hypothyroidism. Unregulated thyroid support formulas lack quality control and scientific backing.
How Does Stress Affect Thyroid Function?
Chronic stress raises cortisol levels which suppress TSH production and reduce T4 to T3 conversion. High cortisol signals the pituitary gland to reduce TSH output. Less TSH means less stimulation of the thyroid. Cortisol also blocks the conversion of T4 into active T3.
Research shows people with stress-related disorders have 30% higher risk of developing autoimmune disease. Veterans with PTSD showed 58% higher chances of autoimmune disease. Chronic stress clearly triggers or worsens autoimmune conditions including Hashimoto's thyroiditis.
Meditation lowers cortisol levels measurably. Deep breathing exercises activate the parasympathetic nervous system. This counters the stress response immediately. Addressing mental health holistically supports thyroid function.
Sleep quality directly impacts stress levels and thyroid function. Aim for 7-9 hours nightly at consistent times. Social connections buffer stress effects powerfully. Setting boundaries prevents stress accumulation and protects limited energy.
What Exercise Benefits Thyroid Health?
Moderate exercise boosts metabolism, reduces inflammation, and regulates hormone levels. Physical activity increases metabolic rate and helps manage weight gain associated with low thyroid function. Exercise reduces systemic inflammation and improves insulin sensitivity.
Walking 30 minutes most days provides excellent benefits without overtaxing the body. Swimming and water aerobics offer low-impact options. Gentle yoga improves flexibility, reduces stress, and supports hormone balance. Light strength training 2-3 times weekly builds muscle and bone density. Those seeking guidance may benefit from holistic medicine approaches to exercise planning.
However, excessive exercise harms thyroid function. Overtraining raises cortisol chronically. Listen to body signals during exercise. Hypothyroid patients often have lower exercise tolerance. Rest days prove just as important as workout days.
How Does Sleep Quality Impact Thyroid Function?
Poor sleep increases cortisol, inflammation, and hormone imbalance. Sleep deprivation elevates cortisol levels measurably. Chronic sleep restriction creates persistently high cortisol which suppresses thyroid function. Inadequate sleep increases systemic inflammation and worsens autoimmune thyroid disease.
Sleep regulates hormone production and release. Growth hormone releases primarily during deep sleep. Leptin and ghrelin, hormones controlling appetite and metabolism, also depend on adequate sleep. For those struggling with sleep disorders, addressing underlying issues becomes critical.
The body follows circadian rhythms aligned with light-dark cycles. Sleeping from approximately 10 PM to 6 AM aligns best with these natural rhythms. Keep bedrooms between 60-67 degrees Fahrenheit. Use blackout curtains or sleep masks. Establish a consistent bedtime routine.
What Environmental Toxins Harm Thyroid Function?
Endocrine-disrupting chemicals interfere with thyroid hormone production and function. Perchlorates contaminate water supplies and block iodine uptake by the thyroid. Polychlorinated biphenyls (PCBs) accumulate in fatty tissues and interfere with thyroid hormone transport. Those interested in environmental medicine can learn more about reducing toxic exposures.
Flame retardants called polybrominated diphenyl ethers (PBDEs) contaminate household dust. Regular dusting and vacuuming with HEPA filters reduce exposure. Bisphenol A (BPA) leaches from plastics. Avoid heating food in plastic containers. Never microwave plastic.
Pesticides and herbicides disrupt endocrine function. Choosing organic produce when possible reduces exposure. Personal care products contain numerous endocrine disruptors including parabens, phthalates, and triclosan. Reading ingredient labels helps identify problematic products.
How Should People Take Thyroid Medication?
Take thyroid medication on an empty stomach 30-60 minutes before eating. Levothyroxine absorbs best in an empty stomach. Food interferes with absorption by 20-40%. Use water only when swallowing thyroid medication. Coffee, juice, and milk reduce absorption.
Consistency in timing matters tremendously. Take medication at the same time every morning. Wait 30-60 minutes before eating or drinking anything besides water. Many medications and supplements interfere with thyroid hormone absorption. Iron supplements reduce absorption significantly. Wait at least four hours after levothyroxine before taking iron, calcium, vitamin D, or magnesium.
What Thyroid Medication Options Exist?
Levothyroxine (synthetic T4) is the most common thyroid medication. The body converts T4 to active T3 as needed. Most people feel well on levothyroxine alone. Synthroid is the most prescribed brand. Generic levothyroxine costs less than brands.
Liothyronine provides synthetic T3 directly. Some people do not convert T4 to T3 efficiently. These patients benefit from adding T3 to their regimen. Combination medications contain both T4 and T3. Armour Thyroid is the most popular natural desiccated thyroid from pig glands.
Those seeking comprehensive functional wellness evaluation may benefit from complete thyroid panels and personalized treatment.
What Tests Diagnose Thyroid Problems?
Complete thyroid testing includes TSH, Free T4, Free T3, and thyroid antibodies. Basic TSH-only tests miss important information about thyroid function.
TSH measures thyroid-stimulating hormone from the pituitary gland. Free T4 measures unbound thyroxine circulating in blood. Free T3 represents the hormone actually available to cells. Thyroid peroxidase (TPO) antibodies appear in most Hashimoto's cases. Thyroglobulin (TG) antibodies also indicate autoimmune attack.
Additional testing supports thyroid health optimization. Vitamin D, B-12, iron, and ferritin reveal nutritional deficiencies. These nutrients support thyroid function. Correcting deficiencies improves symptoms and thyroid health.
When Should Someone Contact A Doctor About Thyroid Symptoms?

Contact a doctor when experiencing persistent fatigue, unexplained weight changes, or temperature sensitivity. Fatigue that rest does not relieve suggests thyroid problems. Unexplained weight gain despite unchanged diet signals possible hypothyroidism. Temperature sensitivity develops in thyroid disorders.
Worsening symptoms despite medication require dose adjustment. Rapid heartbeat or jitteriness suggests excessive medication. Severe fatigue, depression, hair loss, and memory problems need medical evaluation.
Can Pregnancy Affect Thyroid Medication Needs?
Thyroid medication doses typically increase by 30-50% during pregnancy. The growing baby depends entirely on maternal hormones. Untreated hypothyroidism during pregnancy causes miscarriage, preterm birth, and preeclampsia. The baby faces low IQ and developmental delays.
Check TSH and Free T4 as soon as pregnancy confirms. Most doctors recheck every 4-6 weeks during the first half of pregnancy. After delivery, thyroid hormone needs usually decrease. Considering preconception care helps optimize thyroid health before pregnancy begins.
How Do Integrative Medicine Practitioners Treat Thyroid Problems?
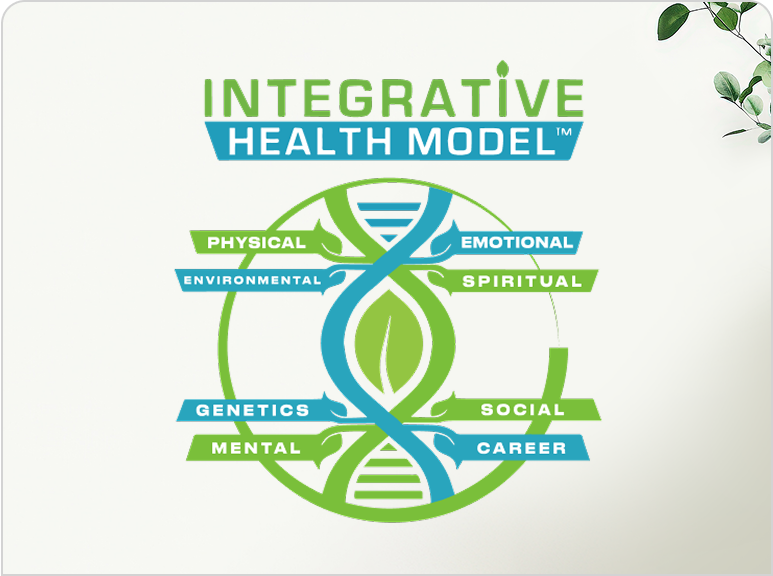
Integrative medicine combines conventional thyroid medication with lifestyle modifications, nutrition, and stress management. Complete evaluation examines all health aspects. Practitioners order Free T4, Free T3, antibodies, and nutritional markers.
Treatment plans combine medication when necessary with natural support methods. Nutrition recommendations address deficiencies and reduce inflammation. Stress management techniques become part of the treatment plan. Practitioners monitor patients closely during treatment adjustments. Learning about the integrative health model helps patients understand this comprehensive approach.
What Daily Habits Support Thyroid Health?
Consistent medication timing, balanced nutrition, stress management, and adequate sleep support optimal thyroid function. Keep thyroid medication on the nightstand. Take it immediately upon waking with water. Breakfast 30-60 minutes after medication provides important nutrients. Include protein, vegetables, and healthy fats.
Drink water consistently throughout the day. Aim for half your body weight in ounces daily. Movement breaks up sedentary periods. Aim for 30 minutes of intentional exercise most days. Stress management requires daily practice through meditation or deep breathing.
Frequently Asked Questions
Can I Stop Taking Thyroid Medication If My Levels Are Normal?
No, normal thyroid levels result from taking medication, not despite it. The medication provides hormones your thyroid cannot produce. Stopping medication causes hormone levels to drop again. Most people with hypothyroidism need medication permanently. Never stop thyroid medication without consulting your doctor first.
How Long Does It Take For Thyroid Medication To Work?
Levothyroxine begins working within a few days but full effects take 4-6 weeks. Most people notice energy improvements within 2-3 weeks. Complete symptom relief often takes 2-3 months as the body adjusts to optimal hormone levels. Your doctor tests thyroid levels after 6-8 weeks to adjust dosage if needed.
Can Stress Cause Hypothyroidism?
Stress alone does not directly cause hypothyroidism but significantly worsens existing thyroid problems. Chronic stress raises cortisol levels which suppress thyroid function. Research shows people with stress-related disorders have 30% higher risk of developing autoimmune thyroid disease. Stress management becomes crucial for anyone with thyroid problems or family history of thyroid disease.
What Foods Should I Avoid With Hypothyroidism?
Avoid taking soy products, high-fiber foods, and calcium or iron supplements within 4 hours of thyroid medication. These interfere with medication absorption. Otherwise, no foods need complete avoidance. Limit excessive raw cruciferous vegetables and reduce sugar and processed foods to decrease inflammation. Most foods are safe in moderate amounts when properly timed around medication.
Is Natural Desiccated Thyroid Better Than Synthetic Medication?
Natural desiccated thyroid works better for some people but not everyone. It contains both T4 and T3 hormones from pig thyroid glands. Some patients report better symptom relief compared to synthetic T4 alone. However, desiccated thyroid has less consistent potency between batches and costs more. Most people do well on synthetic levothyroxine. Work with your doctor to find which medication type suits you best based on symptoms and lab results.
Final Thoughts
Managing thyroid health requires both medication and lifestyle support for most people. Hypothyroidism medication replaces hormones the body cannot produce adequately. Natural approaches like proper nutrition, stress management, exercise, and sleep optimization work alongside medication rather than replacing it.
Subclinical hypothyroidism may reverse in approximately one-third of cases. Overt hypothyroidism and conditions like Hashimoto's disease require lifelong treatment. The thyroid cannot repair itself once significantly damaged.
Comprehensive thyroid testing reveals the complete picture. TSH alone provides insufficient information. Free T4, Free T3, and antibodies guide treatment decisions. Regular monitoring ensures optimal dosing. Most people need adjustments over time.
Lifestyle factors significantly impact thyroid health even with medication. Reducing stress protects thyroid function. Eating nutrient-dense whole foods provides building blocks. Avoiding endocrine-disrupting chemicals reduces toxic burden. Quality sleep supports hormone production and regulation. Appropriate exercise boosts metabolism and mood.
Working with knowledgeable healthcare providers produces the best outcomes. Practitioners who understand both conventional and natural approaches offer comprehensive care. Support exists for those struggling with thyroid symptoms. Family medicine providers offer ongoing care and monitoring. Testing identifies problems early. Treatment begins promptly. The journey to optimal thyroid health is achievable with proper support and dedication.
You May Also Like
.png)
.png)



%201.png)


.png)
.png)



.png)
.png)
.png)
.png)
.png)
.png)
.png)
.png)

.png)
.png)
.png)
.png)

.png)
.png)

.png)
.png)






.png)




.png)
.png)
.png)

.png)

.png)