Do Probiotics Help with Estrogen Dominance?

Yes, probiotics can help with estrogen dominance but they work indirectly through gut health. The gut microbiome helps regulate how your body processes and eliminates excess estrogen. When you take probiotics like Lactobacillus acidophilus, L. rhamnosus, and Bifidobacterium bifidum, they support the estrobolome, the group of gut bacteria that control estrogen metabolism. This helps prevent estrogen buildup and promotes better hormone balance over time.
What Is Estrogen Dominance?
Estrogen dominance occurs when estrogen levels exceed progesterone levels in the body. This hormonal imbalance affects women of all ages and creates symptoms that disrupt daily life.
Recognizing the Symptoms
Women with estrogen dominance experience multiple symptoms including heavy menstrual bleeding, breast tenderness and swelling, and weight gain in hips and abdomen. Mood swings and irritability appear frequently along with fatigue and low energy. Sleep disturbances interrupt rest patterns while brain fog and poor concentration affect work and relationships. Headaches and migraines occur more frequently during hormonal fluctuations.
Primary Causes of Hormone Imbalance
Several factors create estrogen dominance in the female body. Excess body fat produces estrogen through adipose tissue, which converts androgens into estrogen through an enzyme called aromatase. Birth control pills elevate estrogen levels by introducing synthetic hormones that alter natural hormone production. Environmental chemicals mimic estrogen as xenoestrogens from plastics, pesticides, and personal care products bind to estrogen receptors throughout the body.
Poor gut health increases estrogen reabsorption significantly. Gut dysbiosis elevates beta-glucuronidase activity, which frees conjugated estrogen for reabsorption into the bloodstream. Chronic stress depletes progesterone because high cortisol diverts progesterone production toward stress hormone synthesis instead of reproductive hormone balance.
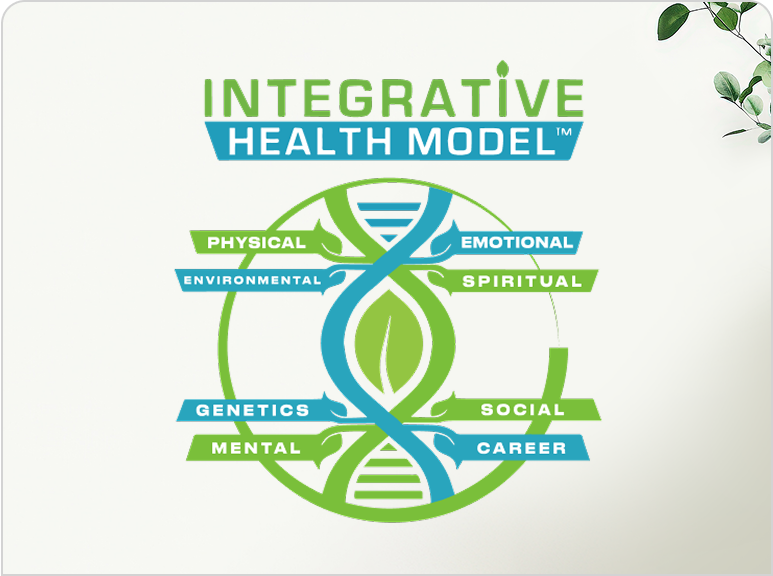
Understanding hormonal imbalances requires looking at multiple body systems working together. The endocrine system connects directly with digestive health, immune function, and detoxification pathways.
How Does the Gut Control Estrogen Levels?
The estrobolome a collection of gut bacteria genes regulates estrogen metabolism through enzymatic activity. These bacteria determine how much estrogen leaves the body versus how much recirculates through the bloodstream.
Understanding the Estrobolome Function
The estrobolome produces beta-glucuronidase, an enzyme that deconjugates estrogen. This process converts inactive, conjugated estrogen into active, free estrogen that the body can reabsorb. Research published in the Journal of Biological Chemistry identified 35 human gut microbial beta-glucuronidase enzymes that reactivate estrogen glucuronides. Specific bacterial families including Bacteroides, Bifidobacterium, Lactobacillus, and Escherichia coli produce this enzyme in varying amounts depending on individual microbiome composition.
The Enterohepatic Circulation Process
Estrogen follows a specific pathway through the body during normal metabolism. The liver conjugates estrogen by attaching glucuronic acid molecules through phase II detoxification processes. Conjugated estrogen enters bile and flows into the intestines where it awaits elimination. Gut bacteria release beta-glucuronidase to deconjugate estrogen at this stage. Free estrogen reabsorbs through intestinal walls into blood circulation, while some deconjugated estrogen exits through fecal elimination.
Impact of Gut Dysbiosis on Hormones
Imbalanced gut bacteria alter estrogen levels in two primary ways. Excessive beta-glucuronidase activity increases estrogen reabsorption by freeing more conjugated estrogen, which raises circulating estrogen and creates dominance symptoms. Low beneficial bacteria reduce proper estrogen elimination because without adequate Lactobacillus and Bifidobacterium strains, the gut cannot regulate estrogen metabolism effectively.
A study in the journal Gut Microbes found that gut microbial beta-glucuronidase acts as a vital regulator in female estrogen metabolism. The research correlates elevated enzyme activity with estrogen-driven diseases including breast cancer and endometriosis. Women with these conditions show distinctly different gut microbiome patterns compared to healthy controls.
How Do Probiotics Balance Estrogen?
Probiotics modulate the estrobolome by altering gut microbiota composition and reducing beta-glucuronidase enzyme production. Specific bacterial strains decrease estrogen reabsorption and support proper hormone elimination through multiple mechanisms.
Reducing Beta-Glucuronidase Activity
Lactobacillus acidophilus supplementation lowers beta-glucuronidase levels in the gut significantly. This probiotic changes the microbial composition of the estrobolome by increasing beneficial bacteria and decreasing pathogenic strains that produce excess enzyme. A clinical study found that L. acidophilus reduced beta-glucuronidase activity by approximately 30%, leading to decreased estrogen reabsorption and improved hormone balance in participants over a 12-week period.
Improving Bowel Transit Time
Regular bowel movements prevent estrogen reabsorption effectively. Probiotics accelerate intestinal transit, reducing the time estrogen spends in the gut environment. Gut bacteria comprise 30% of stool bulk according to digestive health research. Higher probiotic populations increase fecal volume and speed elimination, removing conjugated estrogen before bacteria can deconjugate it and send it back into circulation.
Clinical Research Evidence
Multiple studies demonstrate probiotic effects on estrogen metabolism and related symptoms. A randomized controlled trial published in Journal of Medicinal Food found that women taking Levilactobacillus brevis KABP052 maintained estrogen levels over 12 weeks, while placebo group levels decreased significantly. The study used 111 healthy peri- and postmenopausal women and measured both estradiol and estrone levels throughout the intervention period.
Research in Science Direct showed that four probiotic strains reduced blood glucose, improved depression-like behavior, and enhanced spatial memory in ovariectomized mice without affecting uterine weight. The tested strains included Limosilactobacillus fermentum MG901, Lactiplantibacillus plantarum MG4604, Ligilactobacillus salivarius MG4679, and Lacticaseibacillus reuteri MG5463. These probiotics demonstrated estrogen-like activity without the unfavorable uterine stimulation associated with traditional hormone replacement therapy.
A cross-sectional study using NHANES data revealed associations between probiotic consumption and serum sex steroid hormones in premenopausal women. The analysis included over 1,300 women and found that probiotic users showed different estrogen levels than non-users, supporting the hypothesis that dietary probiotics influence hormone metabolism.
Protection Against Hormone-Related Conditions
Probiotic foods reduce breast cancer risk through positive microbiome changes and better estrogen control according to research published in PMC. The mechanism involves tighter regulation of circulating estrogen levels, which reduces the hormonal stimulus that drives hormone receptor-positive breast cancer growth. Lactobacillus gasseri suppresses endometriosis through immune system modulation as demonstrated in multiple studies on estrogen-driven diseases.
Many women seek naturopathic treatment for hormonal imbalance that addresses root causes rather than just symptoms. Probiotics represent one evidence-based tool in comprehensive hormone management.
Which Probiotic Strains Work Best for Hormone Balance?
Lactobacillus and Bifidobacterium species provide the strongest evidence for hormone regulation. Research identifies specific strains that reduce estrogen dominance symptoms through documented mechanisms.
Lactobacillus Acidophilus La-14
Lactobacillus acidophilus La-14 supports urinary tract health and reduces beta-glucuronidase activity in the gut. Clinical trials show L. acidophilus La-14 combined with L. rhamnosus HN001 increased Lactobacillus populations in the vaginal microbiome within 15 days of supplementation. This strain demonstrates multiple benefits including lower beta-glucuronidase enzyme production, improved digestive function, and reduced bloating and gas. The strain-specific designation La-14 indicates research backing for this particular genetic variant.
Lactobacillus Rhamnosus HN001
Lactobacillus rhamnosus HN001 maintains vaginal pH and prevents urinary tract infections through acidification of the vaginal environment. Studies on menopausal mice showed this strain protected against bone loss, leaky gut, and inflammation without unfavorable uterine stimulation. The research demonstrated benefits including enhanced vaginal microbiome health, stronger immune defenses, and better bone density maintenance during periods of declining estrogen production.
Lactobacillus Plantarum ROSELL-A
Lactobacillus plantarum ROSELL-A demonstrates significant effects on vaginal health in clinical research. A 45-day trial showed 95% improvement in healthy vaginal flora levels among participants taking this specific strain. Benefits include enhanced gut barrier function through tight junction protein expression, anti-inflammatory properties that reduce systemic inflammation markers, and better skin health through the gut-skin axis connection.
Lactobacillus Reuteri MG5463
Lactobacillus reuteri MG5463 prevented ovariectomy-induced bone loss in animal studies examining menopause effects. This strain increased cortical bone mineral density and bone volume fraction in research subjects, suggesting potential applications for postmenopausal bone health. Benefits include bone health protection during hormonal transitions and reduced systemic inflammation throughout the body.
Bifidobacterium Species for Digestive Health
Bifidobacterium lactis and Bifidobacterium longum support digestive regularity and strengthen intestinal barrier integrity. Multiple Bifidobacterium species reinforce gut barrier function, preventing toxin reabsorption that would otherwise burden the liver. These strains improve bowel movement frequency, strengthen gut lining through mucin production, and enhance nutrient absorption in the small intestine.
Women exploring functional medicine approaches often discover that probiotic selection matters more than generic supplementation. Strain-specific research guides effective interventions.
What Foods Support the Estrobolome?
High-fiber foods and fermented products provide prebiotics and probiotics that balance gut bacteria. Diet directly influences estrobolome composition and function through substrate availability and bacterial colonization.
Dietary fiber binds to conjugated estrogen in the intestines and promotes fecal excretion. Adults need 25-30 grams of fiber daily, but most consume less than 15 grams according to nutritional surveys. Fiber sources include vegetables like broccoli, carrots, and Brussels sprouts which provide both soluble and insoluble fiber types. Fruits including berries, apples, and pears contain pectin and other fermentable fibers. Legumes including lentils, chickpeas, and black beans offer resistant starch and high fiber content. Whole grains including oats, quinoa, and brown rice provide beta-glucan and other beneficial compounds.
Fermented foods contain billions of beneficial bacteria that colonize the gut microbiome. Regular consumption maintains healthy estrobolome diversity by introducing varied bacterial strains. Plain yogurt with live active cultures provides minimum 1 billion CFU per serving depending on brand and freshness. Kefir contains multiple Lactobacillus and yeast strains in a drinkable format with higher probiotic counts than yogurt. Raw sauerkraut with Lactobacillus plantarum offers both probiotics and fiber from cabbage. Kimchi provides Lactobacillus sakei and L. plantarum along with beneficial compounds from garlic and ginger. Kombucha offers various bacterial and yeast species though sugar content varies by brand.
Cruciferous vegetables contain indole-3-carbinol and sulforaphane compounds that enhance liver estrogen metabolism. These vegetables support phase I and phase II detoxification pathways that convert and conjugate estrogen. Cruciferous options include broccoli, cauliflower, kale, cabbage, and bok choy. Consuming these vegetables 3-4 times weekly provides adequate compounds for enhanced estrogen metabolism.
Research shows that dietary patterns affect gut microbiome composition within 24-48 hours of dietary changes. However, stable microbiome shifts require several weeks to months of consistent dietary patterns. The Mediterranean diet provides high fiber, omega-3 fatty acids, and polyphenols that support gut health and hormone balance. This eating pattern correlates with improved gut microbiome diversity and reduced inflammation markers.
For comprehensive support, many practitioners recommend combining dietary changes with professional guidance through functional wellness programs that address multiple factors simultaneously.
How Should You Take Probiotics for Estrogen Balance?
Choose multi-strain probiotic supplements containing 10-50 billion CFU of researched Lactobacillus and Bifidobacterium strains. Consistent daily use provides optimal results for hormone balance.
Selecting the Right Probiotic Formula
Colony-forming units indicate live bacteria quantity in each dose. Effective probiotics contain 5-50 billion CFU per dose depending on formulation and intended use. Strain names matter significantly look for specific identifiers like "Lactobacillus acidophilus La-14" rather than generic species names without strain designation. Products listing strain-specific identifiers provide transparency about which bacteria the supplement contains and whether research supports those particular strains.
Optimal Timing and Delivery Methods
Delayed-release or enteric-coated capsules protect bacteria from stomach acid and deliver them to intestines alive. Powder forms mix into cold beverages or foods but heat kills probiotic bacteria. Take probiotics with meals or within 30 minutes after eating because food buffers stomach acid and improves bacterial survival rates through the digestive system.
Storage Requirements and Shelf Life
Some probiotics require refrigeration to maintain potency throughout shelf life. Shelf-stable formulations use lyophilization technology that preserves bacteria at room temperature. Check product labels and follow storage instructions precisely because heat and moisture destroy probiotic viability. Store supplements in cool, dry locations away from direct sunlight and humid environments.
Timeline for Expected Results
The timeline for results varies by individual and baseline health status. During weeks 1-2, digestive changes appear including more regular bowel movements and possible temporary gas or bloating. These symptoms indicate gut microbiome shifts beginning. During weeks 4-8, reduced PMS symptoms, better sleep quality, and more stable moods become noticeable. The gut has had time to build beneficial bacteria populations. During weeks 12-24, lighter periods, improved skin clarity, easier weight management, and fewer hormonal symptoms develop. Individual responses vary based on baseline gut health, diet quality, and symptom severity.
What Other Supplements Support Estrogen Balance?

Calcium D-glucarate and DIM complement probiotic therapy by blocking beta-glucuronidase and supporting liver detoxification. These supplements enhance estrogen elimination through different mechanisms than probiotics.
Calcium D-Glucarate for Enzyme Inhibition
Calcium D-glucarate inhibits beta-glucuronidase enzyme activity, keeping estrogen conjugated for elimination through fecal excretion. Typical doses range from 500-1500 mg daily depending on individual needs and beta-glucuronidase levels. Research shows calcium D-glucarate blocks beta-glucuronidase, reducing deconjugation of estrogen and supporting proper excretion of estrogen metabolites through the intestinal tract.
DIM for Beneficial Estrogen Metabolism
DIM contains concentrated compounds from cruciferous vegetables extracted and standardized. This supplement promotes beneficial estrogen metabolism by increasing 2-hydroxyestrone, a protective estrogen metabolite, while decreasing 16-alpha-hydroxyestrone, a problematic metabolite associated with increased cancer risk. Standard DIM doses range from 100-300 mg daily. Start with lower doses and increase gradually to assess tolerance and response.
Additional Supportive Nutrients
B vitamins including B6, B12, and folate support methylation pathways that convert estrogen metabolites into safer forms for elimination. Magnesium acts as a cofactor for over 300 enzymatic reactions, including detoxification processes that handle hormone metabolism. N-acetyl cysteine provides cysteine for glutathione synthesis, the liver's primary antioxidant system used in phase II detoxification. Milk thistle containing silymarin protects hepatocytes and enhances liver regeneration capacity.
Protein Requirements for Hormone Production
Adequate protein intake supports hormone synthesis and liver detoxification processes. Women need approximately 0.8-1.2 grams of protein per kilogram of body weight daily for optimal hormone production. Protein sources including eggs, fish, poultry, legumes, and dairy provide amino acids necessary for hormone production and conjugation reactions in the liver.
Addressing digestive issues often improves hormone balance because proper digestion and elimination remove excess hormones effectively.
When Should You See a Healthcare Provider?
Consult a healthcare provider if symptoms persist after 12 weeks of natural interventions or if severe symptoms interfere with daily activities. Professional testing identifies underlying causes and guides treatment decisions.
Hormone Testing Options
The DUTCH Complete Test measures estrogen metabolites, progesterone, cortisol, and organic acids through dried urine samples. This test shows how the body metabolizes estrogen and which pathways dominate. Serum hormone panels through blood tests measure estradiol, estrone, progesterone, testosterone, and thyroid hormones at specific time points in the menstrual cycle. Comprehensive digestive stool analysis reveals gut microbiome composition, beta-glucuronidase levels, and digestive function markers including inflammatory markers and immune function.
Testing provides objective data about hormone levels and gut health, enabling targeted interventions based on individual biochemistry. Generic approaches often fail because hormone imbalances stem from different root causes in different women.
Symptoms Requiring Medical Attention
Seek immediate medical attention for menstrual bleeding exceeding 80 ml per cycle, which typically means soaking through protection hourly. New breast lumps or changes in breast tissue require evaluation. Postmenopausal bleeding always warrants investigation. Severe pelvic pain that limits normal activities needs assessment. Symptoms worsening despite treatment indicate the need for different approaches.
Working with Integrative Practitioners
These symptoms may indicate conditions including endometriosis, uterine fibroids, polycystic ovary syndrome, or hormone-sensitive cancers requiring medical management. Naturopathic doctors can recommend specific probiotic strains, dietary modifications, and lifestyle interventions based on individual test results and health history.
Many women benefit from integrative health approaches that combine conventional diagnostics with natural therapies for comprehensive care.
How Do Lifestyle Factors Affect Estrogen Dominance?

Stress management, regular exercise, adequate sleep, and reduced toxin exposure significantly impact estrogen metabolism. These factors work synergistically with probiotics for optimal hormone balance.
Managing Stress and Cortisol Levels
Chronic stress elevates cortisol, which inhibits progesterone production and creates relative estrogen dominance. Cortisol and progesterone share the same precursor molecule called pregnenolone, so high stress depletes progesterone reserves for reproductive hormone balance. Daily meditation for 10-20 minutes reduces cortisol levels measurably. Deep breathing exercises activate the parasympathetic nervous system. Regular yoga practice combines movement with stress reduction. Adequate social support buffers stress responses.
Exercise for Hormone Metabolism
Regular physical activity lowers circulating estrogen levels through multiple mechanisms. Exercise increases hepatic blood flow, enhancing liver detoxification capacity for hormone metabolism. Physical activity also reduces body fat, decreasing aromatase enzyme activity that converts androgens to estrogen. Aim for 150 minutes of moderate-intensity exercise weekly plus two strength training sessions. Studies show this exercise volume significantly impacts hormone balance by improving insulin sensitivity and reducing inflammation.
Sleep Quality and Hormonal Balance
Poor sleep disrupts all hormonal systems including the hypothalamic-pituitary-gonadal axis. The hypothalamic-pituitary-gonadal axis requires 7-9 hours of quality sleep nightly for proper function. Sleep deprivation increases cortisol, reduces growth hormone secretion, and impairs insulin sensitivity all factors that worsen estrogen dominance. Consistent sleep schedules and dark, cool sleeping environments support hormone production.
Reducing Environmental Toxin Exposure
Xenoestrogens from plastics including BPA and phthalates add to total estrogen burden. Pesticides including atrazine and DDT persist in the environment and food chain. Personal care products containing parabens and triclosan expose users to endocrine disruptors daily. Minimize exposure by using glass or stainless steel food containers, choosing organic produce when possible, selecting paraben-free personal care products, avoiding plastic water bottles, and using natural cleaning products.
Understanding how environmental factors impact health helps women make informed choices about daily exposures.
What Role Does Liver Function Play?
The liver performs phase I and phase II detoxification to metabolize and conjugate estrogen for elimination. Optimal liver function prevents estrogen accumulation in tissues and circulation.
Phase I and Phase II Detoxification Pathways
Phase I metabolism involves cytochrome P450 enzymes that hydroxylate estrogen, creating metabolites including 2-hydroxyestrone, 4-hydroxyestrone, and 16-alpha-hydroxyestrone. Each metabolite has different biological activity and cancer risk profiles. Phase II conjugation uses glucuronidation, sulfation, and methylation pathways to attach molecules to estrogen metabolites, making them water-soluble for excretion through bile and urine. Poor liver function slows both phases, allowing estrogen and toxic metabolites to accumulate in body tissues.
Essential Nutrients for Liver Health
Several nutrients enhance hepatic estrogen metabolism effectively. B vitamins including B6, B12, and folate support methylation pathways that convert estrogen metabolites into safer forms. Magnesium acts as a cofactor for enzymatic reactions throughout detoxification. N-acetyl cysteine provides cysteine for glutathione synthesis, which the liver uses extensively. Milk thistle containing silymarin protects hepatocytes and enhances liver regeneration after damage.
Impact of Alcohol on Detoxification
Alcohol consumption directly impairs liver detoxification capacity. The liver prioritizes alcohol metabolism over hormone metabolism, creating a backlog of estrogen and other compounds awaiting processing. Chronic alcohol use damages hepatocytes and reduces phase II conjugation capacity. Women metabolize alcohol differently than men, experiencing greater liver impact from equivalent consumption.
Can Probiotics Help During Menopause?
Probiotics support hormone balance during perimenopause and postmenopause by modulating the estrobolome and reducing menopause symptoms. Research demonstrates specific benefits for postmenopausal women experiencing hormonal transitions.
Microbiome Changes During Menopause
Gut microbiota composition differs between premenopausal and postmenopausal women significantly. Lower estrogen levels alter microbial diversity and affect beta-glucuronidase activity in the gut. A study published in Maturitas found that postmenopausal women have distinct gut microbiome patterns compared to premenopausal women, affecting estrogen metabolism and related health outcomes including cardiovascular health and bone density.
Probiotic Benefits for Menopausal Health
Research shows probiotics help manage bone density loss by increasing calcium absorption and producing vitamin K2, which supports bone health. Probiotics reduce vaginal atrophy through Lactobacillus strains that maintain vaginal pH and reduce infection risk despite lower estrogen levels. Certain probiotic strains improve insulin sensitivity and reduce weight gain associated with menopause. Psychobiotics influence the gut-brain axis, reducing anxiety and depression symptoms common during hormonal transitions.
Menopausal women seeking natural support often explore anti-aging medicine approaches that address multiple systems simultaneously for comprehensive wellness.
How Does Estrogen Dominance Affect Other Health Conditions?
Estrogen dominance increases risk for endometriosis, uterine fibroids, polycystic ovary syndrome, and hormone-sensitive cancers. Proper estrogen balance through gut health interventions may reduce these risks.
Connection to Endometriosis
Endometriosis affects approximately 10% of reproductive-age women globally. This condition creates endometrial-like tissue growth outside the uterus, driven primarily by estrogen stimulation. Research demonstrates correlations between gut microbiota dysbiosis and endometriosis severity. Women with endometriosis show elevated beta-glucuronidase activity and distinct gut microbiome patterns compared to healthy controls, suggesting gut-hormone connections in disease development.
Impact on Polycystic Ovary Syndrome
Polycystic ovary syndrome creates both elevated androgens and relative estrogen dominance simultaneously. Probiotic administration improves PCOS symptoms including insulin resistance, high testosterone, inflammation, and metabolic markers. A clinical trial found probiotics significantly reduced BMI by average 2.1 kg/m², serum insulin by average 3.5 mU/L, and blood lipid levels in women with PCOS over 12 weeks of supplementation.
Breast Cancer Risk Factors
Elevated circulating estrogen increases breast cancer risk through multiple mechanisms. The estrobolome influences this risk through beta-glucuronidase activity that controls estrogen reabsorption. An estrobolome enriched in beta-glucuronidase enzymes promotes estrogen metabolite deconjugation, resulting in greater reabsorption of free estrogens and higher risk of hormone receptor-positive cancers according to research published in the Journal of the National Cancer Institute.
What Are Common Mistakes with Probiotic Use?
Taking probiotics inconsistently, choosing wrong strains, or expecting immediate results undermines effectiveness. Avoiding these mistakes improves outcomes significantly.
Inconsistent Supplementation Patterns
Probiotic effects require consistent daily use over extended periods. Sporadic supplementation fails to establish stable gut microbiome changes because beneficial bacteria need regular reinforcement to compete with existing microbiota. The gut microbiome reaches new equilibrium states after several weeks to months of consistent probiotic supplementation according to microbiome research.
Ignoring Prebiotic Fiber Intake
Probiotics need prebiotics including fermentable fibers to thrive in the gut environment. Taking probiotics without dietary fiber reduces their effectiveness substantially. Prebiotic sources including garlic, onions, asparagus, bananas, and whole grains feed beneficial bacteria and enhance probiotic colonization rates in the intestinal tract.
Improper Antibiotic Timing
Antibiotics kill both harmful and beneficial bacteria indiscriminately. Taking probiotics during antibiotic treatment reduces effectiveness because antibiotics destroy probiotic bacteria. Take probiotics 2-3 hours apart from antibiotic doses, and continue probiotic supplementation for 2-4 weeks after completing antibiotics to restore gut microbiome diversity and function.
Frequently Asked Questions
How long does it take for probiotics to balance hormones?
Probiotics require 12-24 weeks of consistent daily use to produce noticeable hormone balance improvements. Initial digestive changes appear within 2-4 weeks, while hormonal symptoms including PMS, mood swings, and cycle regularity improve after 8-12 weeks of supplementation. Individual timelines vary based on baseline gut health, diet quality, and severity of estrogen dominance.
Can probiotics make estrogen dominance worse?
Probiotics do not worsen estrogen dominance when taken at appropriate doses with researched strains. Some women experience temporary bloating or digestive changes during the first 1-2 weeks as gut bacteria populations shift. These symptoms resolve as the microbiome adjusts. Probiotics that increase estrogen reabsorption have not been documented in clinical research.
What is the best time to take probiotics for hormone balance?
Take probiotics with meals or within 30 minutes after eating for optimal bacterial survival through stomach acid. Morning or evening timing produces similar results provided consistency remains daily. Some women prefer morning doses to establish routine adherence, while others choose evening doses with dinner. Consistency matters more than specific timing.
Do probiotics help with weight gain from estrogen dominance?
Probiotics support weight management by improving insulin sensitivity, reducing inflammation, and enhancing metabolism according to research from the National Institutes of Health. Specific strains including Lactobacillus gasseri and Lactobacillus rhamnosus reduce body weight and waist circumference in clinical trials. Probiotics work best combined with high-fiber diet and regular exercise for weight management.
Should I take probiotics if I'm on birth control?
Women taking birth control can safely take probiotics for hormone balance support. Birth control elevates estrogen levels, making probiotic support for estrogen elimination potentially beneficial. Probiotics do not interfere with birth control effectiveness. Continue both supplements and contraceptives as prescribed while monitoring symptoms for improvements in PMS, bloating, and mood changes.
Final Thoughts
Probiotics offer evidence-based support for estrogen dominance by modulating gut bacteria that control hormone metabolism. Specific Lactobacillus and Bifidobacterium strains reduce beta-glucuronidase activity, decrease estrogen reabsorption, and improve hormone-related symptoms through documented mechanisms.
Combining probiotics with high-fiber diet, fermented foods, stress management, regular exercise, and reduced toxin exposure creates comprehensive hormone balance. Testing hormone levels and gut microbiome composition through qualified providers enables targeted interventions based on individual biochemistry.
Women experiencing persistent symptoms despite natural approaches should consult healthcare providers. Professional evaluation identifies underlying conditions requiring medical treatment beyond natural interventions alone.
Consistent probiotic use for 12-24 weeks produces measurable improvements in estrogen metabolism and symptom reduction. Start with researched strains containing Lactobacillus acidophilus, L. rhamnosus, and Bifidobacterium species. Maintain daily supplementation and support gut health through diet and lifestyle modifications.
Take action by selecting a quality multi-strain probiotic from reputable manufacturers. Combine with increased dietary fiber reaching 25-30 grams daily, reduced alcohol consumption, and stress management practices. Monitor symptoms through journaling and consider hormone testing to track progress objectively.
Proper estrogen balance improves energy, mood, sleep quality, menstrual regularity, and long-term health outcomes. The gut-hormone connection provides a powerful intervention point for natural hormone regulation without pharmaceutical hormone replacement.
You May Also Like
.png)
.png)



%201.png)


.png)
.png)



.png)
.png)
.png)
.png)
.png)
.png)
.png)
.png)

.png)
.png)
.png)
.png)

.png)
.png)

.png)
.png)






.png)




.png)
.png)
.png)

.png)

.png)