Functional Medicine Approaches to Treating Depression

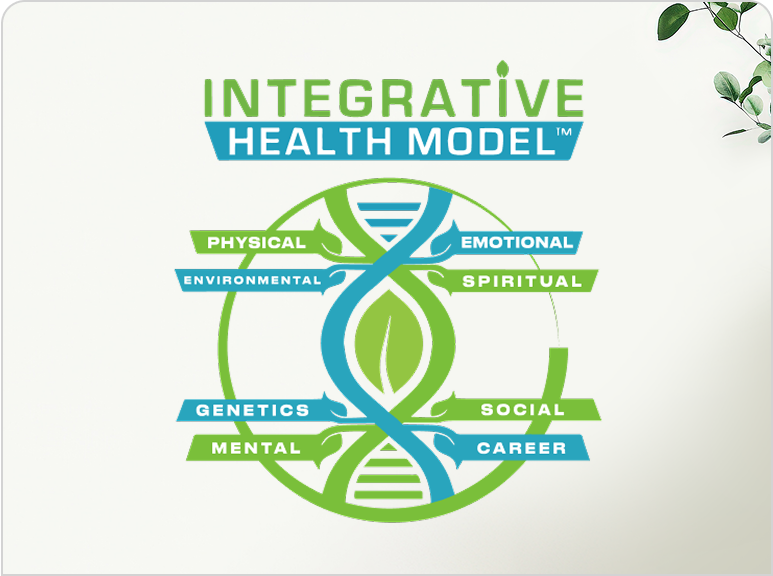
Functional medicine can help treat depression but it does so by addressing the root causes rather than just symptoms. Practitioners look at hormone imbalances, gut health, nutrient deficiencies, inflammation, and stress response to identify what’s disrupting mood regulation. Treatments may include diet changes, targeted supplements, stress management, and lifestyle adjustments alongside traditional care. This whole-body approach supports long-term emotional and mental balance.
Over 47 million Americans currently experience depression. The CDC reports depression rates increased from 8.2% in 2013-2014 to 13.1% by 2023. Young adults face the highest rates, with 26.7% affected in 2025.
How Does Functional Medicine Differ from Conventional Depression Treatment?
Functional medicine identifies specific biological imbalances causing depression rather than prescribing standard medications for symptom management.
Conventional psychiatry uses the DSM-5 to diagnose based on symptoms alone. Patients receive antidepressants targeting neurotransmitter levels. This approach overlooks digestive health, immune function, and metabolic factors that contribute to mood disorders.
Research shows that only 25% of people with depression actually have low neurotransmitter levels, while others show elevated levels. The chemical imbalance theory fails to explain depression for most patients. Studies from 2025 identified 700 different genetic variations and 300 specific genes linked to depression, proving this condition stems from multiple causes.
Naturopathic medicine practitioners order comprehensive lab tests including nutrient panels, hormone assessments, inflammatory markers, gut microbiome analysis, food sensitivity panels, and genetic testing for variants like MTHFR and GAD. Treatment plans address personal biochemistry through diet modifications, targeted supplements, lifestyle changes, and stress reduction.
The goal focuses on restoring normal function rather than suppressing symptoms. Practitioners spend time understanding medical history, environmental exposures, dietary patterns, sleep quality, stress levels, and relationship dynamics. This information reveals patterns that standard psychiatric evaluations miss.
What Causes Depression According to Functional Medicine?
Depression results from multiple interconnected factors including gut dysbiosis, chronic inflammation, blood sugar imbalance, nutrient deficiencies, hormonal disruption, and environmental toxins.
The Gut-Brain Connection
The gut-brain axis connects the digestive system and central nervous system through neural, endocrine, and immune pathways. About 90% of serotonin production occurs in the gut, not the brain. This fact alone challenges traditional psychiatric models that focus exclusively on brain chemistry.
Gut dysbiosis means an imbalance in intestinal bacteria composition. Studies show people with major depressive disorder have different gut microbiome patterns compared to healthy individuals. Beneficial bacteria like Lactobacillus and Bifidobacterium decrease while inflammatory species increase.
Leaky gut allows lipopolysaccharides and other endotoxins to enter the bloodstream, triggering systemic inflammation. This inflammation affects brain function and neurotransmitter production through multiple mechanisms. The vagus nerve transmits signals between gut and brain, creating bidirectional communication that influences mood, cognition, and behavior.
Blood Sugar and Metabolic Dysfunction
Blood sugar dysregulation affects brain function and mood stability. Insulin influences neuronal circuitry formation and synaptic plasticity. Insulin resistance creates a pro-inflammatory state affecting mental health. Obesity correlates with depression through elevated inflammatory cytokines. People with metabolic syndrome show higher rates of depressive symptoms.
Stress and HPA Axis Dysfunction
The hypothalamic-pituitary-adrenal axis regulates stress response. Chronic stress keeps this system activated, releasing excess cortisol. Elevated cortisol damages the hippocampus and prefrontal cortex over time. HPA axis dysfunction also affects thyroid function, creating symptoms like fatigue, weight changes, and mood problems.
Nutrient Deficiencies and Brain Function
More than 20 nutrient deficiencies link to depression. Vitamin D levels below optimal range correlate strongly with depressive symptoms. B vitamins including B6, B12, and folate support neurotransmitter synthesis. Omega-3 fatty acids EPA and DHA reduce neuroinflammation. Magnesium supports GABA production and nervous system regulation. Zinc and copper must maintain proper balance for neurotransmitter function. Amino acids like tryptophan and tyrosine serve as neurotransmitter precursors.
Chronic Inflammation
Depressed patients show elevated inflammatory markers including interleukin-6, tumor necrosis factor-alpha, and C-reactive protein. Inflammation sources include processed food consumption, intestinal permeability, chronic stress, environmental toxin exposure, sedentary behavior, and sleep deprivation. Neuroinflammation disrupts neurotransmitter metabolism and impairs neuroplasticity.
Environmental Toxins
Indoor mold exposure triggers inflammatory responses leading to cognitive symptoms including depression. Mycotoxins from mold affect mitochondrial function and neurotransmitter production. Air pollution causes neuroinflammation, particularly affecting individuals exposed during childhood. Studies show ambient particulate matter increases depression risk significantly.
Chronic Infections
Several infections associate with depression including Lyme disease, toxoplasma gondii, West Nile virus, and clostridium difficile. The pathogen-host defense theory suggests depressive behaviors evolved as responses to infection. Chronic infections maintain inflammatory states affecting brain function through immune activation.
What Tests Does Functional Medicine Use for Depression?
Functional medicine practitioners order comprehensive lab panels measuring nutrient levels, hormones, inflammation markers, gut health, and genetic variants to identify specific depression causes.
Standard testing includes complete blood count, metabolic panel, vitamin D levels, complete thyroid panel with TSH, Free T3, Free T4, Reverse T3, and thyroid antibodies. Sex hormones including estrogen, progesterone, testosterone, and DHEA require measurement. Cortisol testing uses 4-point salivary collection or DUTCH test for comprehensive adrenal function assessment.
Inflammatory markers including hs-CRP, homocysteine, and ferritin reveal immune system activation. Methylation panels measure homocysteine, B12, folate, and methionine levels. Comprehensive stool analysis examines microbiome diversity, pathogenic bacteria, parasites, and digestive function markers.
Organic acids testing reveals metabolic markers, neurotransmitter metabolites, and mitochondrial function status. Food sensitivity panels measure IgG, IgE, and IgG4 reactions to common foods. Heavy metal testing through blood or urine analysis identifies toxic element burden.
Genetic testing examines MTHFR, COMT, MAO-A, and other variants affecting neurotransmitter metabolism. The SLC5A4 gene helps transport serotonin between gut and brain. MTHFR gene polymorphisms affect folate metabolism and methylation pathways. GAD gene changes decrease glutamate conversion to GABA, potentially causing major depressive disorder.
Results guide personalized treatment protocols addressing specific imbalances. Someone with vitamin D deficiency, gut dysbiosis, and elevated cortisol receives different interventions than someone with MTHFR variants, low omega-3s, and thyroid dysfunction.
What Dietary Changes Help Depression?

An anti-inflammatory whole foods diet reduces depression symptoms by supporting gut health, stabilizing blood sugar, and providing essential nutrients for neurotransmitter production.
Foods That Support Mental Health
Fatty fish like salmon, sardines, and mackerel provide EPA and DHA omega-3s that reduce brain inflammation. Leafy greens including spinach, kale, and Swiss chard contain folate and magnesium. Fermented foods like yogurt, kefir, sauerkraut, and kimchi supply beneficial probiotics that support gut-brain communication.
Colorful vegetables including bell peppers, carrots, and beets provide antioxidants that protect brain cells. Nuts and seeds like walnuts, pumpkin seeds, and flaxseeds offer omega-3s and minerals. Berries including blueberries, strawberries, and blackberries contain polyphenols that enhance cognitive function. Quality protein from grass-fed meat, pastured eggs, and legumes supplies amino acids needed for neurotransmitter synthesis.
Research on Diet and Depression
Research shows Mediterranean diet patterns correlate with lower depression rates. One 2017 study found dietary intervention reduced depressive symptoms significantly compared to social support alone. The SMILES trial demonstrated that 32% of participants achieved remission through dietary changes.
Ultra-processed foods including packaged snacks, frozen meals, and fast food increase inflammation throughout the body and brain. Added sugars cause blood sugar spikes and crashes affecting mood stability. Refined grains like white bread, pasta, and crackers lack nutrients and fiber needed for optimal brain function. Industrial seed oils including corn, soybean, and canola oils contain pro-inflammatory omega-6 fatty acids. Artificial additives including preservatives, colors, and sweeteners may affect neurotransmitter function.
Key Nutrients and Recommended Doses
Tryptophan from turkey, eggs, and cheese converts to serotonin in the brain. Tyrosine from chicken, almonds, and avocados serves as precursor to dopamine. B6 functions as cofactor for neurotransmitter synthesis at doses of 50-100 mg daily. B12 supports methylation at 1000-2000 mcg daily. Folate in methylfolate form works best for those with MTHFR variants at 400-800 mcg daily.
Magnesium in glycinate form absorbs best at 300-400 mg daily. Zinc requires 15-30 mg daily with copper balance. Vitamin D3 doses of 2000-5000 IU daily adjust based on blood levels. Omega-3s provide 1-2 grams EPA+DHA daily for optimal brain support.
How Does Gut Health Affect Depression?
Gut microbiome imbalances directly influence brain function through the vagus nerve, immune signaling, neurotransmitter production, and metabolic pathways.
The enteric nervous system contains over 500 million neurons that communicate with the central nervous system. This gut brain produces neurotransmitters, responds to stress hormones, and influences emotional states independently of conscious thought.
The vagus nerve transmits signals between gut and brain stem constantly. Studies show vagotomy blocks antidepressant effects of certain probiotics, proving this nerve plays essential roles in mood regulation. Vagal tone measured through heart rate variability correlates with depression severity.
Gut bacteria produce short-chain fatty acids including butyrate, propionate, and acetate through fiber fermentation. These metabolites cross the blood-brain barrier and affect neuronal function. Altered SCFA levels appear in depressed patients compared to healthy controls. Butyrate particularly supports brain-derived neurotrophic factor production.
Gut microbes synthesize GABA, serotonin, dopamine, and norepinephrine directly. Bacterial species including Lactobacillus and Bifidobacterium produce these compounds that influence mood and cognition. The gut manufactures more neurotransmitters than the brain, making microbial balance critical for mental health.
Gut dysbiosis increases intestinal permeability, allowing lipopolysaccharides into circulation. These endotoxins activate inflammatory cascades through toll-like receptor signaling. Cytokines including IL-6 and TNF-alpha travel to the brain, triggering neuroinflammation that disrupts neurotransmitter metabolism.
Gut microbiota influence the kynurenine pathway that metabolizes tryptophan. Dysregulation produces neurotoxic metabolites including quinolinic acid instead of converting tryptophan to serotonin. This shift contributes to depressive symptoms through NMDA receptor activation and oxidative stress.
Specific probiotic strains show antidepressant effects in clinical trials. Lactobacillus rhamnosus reduces anxiety-like behavior and modulates GABA receptors in animal studies. Bifidobacterium longum decreases inflammatory cytokines and improves stress response. Lactobacillus helveticus combined with B. longum reduces psychological distress in human trials. Lactobacillus plantarum supports intestinal barrier integrity and reduces inflammation.
Addressing digestive issues through functional medicine protocols often produces significant mood improvements within weeks. Removing inflammatory foods, adding fermented foods, supplementing with probiotics, and healing intestinal permeability creates favorable conditions for neurotransmitter production.
What Lifestyle Changes Reduce Depression?
Regular exercise, consistent sleep schedules, stress management practices, social connection, and nature exposure significantly reduce depressive symptoms through multiple biological pathways.
Exercise and Physical Activity
Physical activity reduces depression as effectively as antidepressants in multiple studies. Aerobic exercise for 30-45 minutes, 3-5 times weekly at moderate intensity produces measurable improvements. Resistance training 2-3 sessions weekly improves strength and confidence while supporting metabolic health. Yoga combines movement, breathing, and nervous system regulation in single practice. Walking 10,000 steps daily supports both metabolic and mental health through consistent low-intensity movement.
Exercise increases brain-derived neurotrophic factor, promotes neurogenesis in the hippocampus, reduces systemic inflammation, and improves mitochondrial function. The initial inflammatory response triggers compensatory anti-inflammatory mechanisms that benefit long-term health.
Sleep Optimization
Consistent sleep schedules with same bedtime and wake time daily, including weekends, regulate circadian rhythms. Darkness through blackout curtains, removing electronics, and using only red light after sunset supports melatonin production. Temperature between 65-68°F creates optimal sleep conditions. Timing matters with no caffeine after 2 PM and finishing eating 3 hours before bed. Wind-down routines including reading, gentle stretching, or warm baths 60-90 minutes before sleep prepare the nervous system for rest.
Sleep deprivation impairs emotional regulation and increases inflammatory markers significantly. Seven to nine hours nightly supports mental health through restoration of brain function, consolidation of memories, and clearance of metabolic waste products.
Stress Management Techniques
Managing stress through holistic approaches produces measurable physiological changes. Meditation for 10-20 minutes daily reduces cortisol and increases GABA production. Deep breathing using 4-7-8 pattern activates parasympathetic nervous system response. Time in nature for 20 minutes outdoors reduces stress markers including cortisol and blood pressure. Social connection through regular interaction lowers inflammatory cytokines and improves overall health outcomes.
Studies show mind-body practices reduce both depressive symptoms and inflammatory markers including CRP. One pilot study found functional therapy combining psychotherapy, mind-body techniques, and lifestyle changes reduced depression scores and CRP levels significantly.
Environmental Detoxification
Environmental toxin reduction decreases inflammatory burden affecting brain function. Water filtration removes chlorine, fluoride, and heavy metals from drinking water. Organic foods reduce pesticide exposure, particularly important for produce on the dirty dozen list. Air purification using HEPA filters removes particulate matter and volatile organic compounds. Mold remediation addresses water damage and humidity issues that promote toxic growth. Reducing plastics by using glass containers and avoiding heating plastic prevents endocrine disruption.
What Supplements Support Depression Recovery?
Targeted supplements including omega-3 fatty acids, vitamin D, B-complex vitamins, magnesium, and specific amino acids address nutritional deficiencies contributing to depression.
Essential Fatty Acids
Omega-3 fatty acids at 1-2 grams daily, particularly EPA, show significant antidepressant effects in meta-analyses. Studies demonstrate doses above 1000 mg EPA daily produce better results than lower doses. Fish oil supplements should provide third-party testing for purity and potency.
Vitamins and Minerals
Vitamin D3 at 2000-5000 IU daily corrects deficiency linked to depression severity. Studies show supplementation improves mood when baseline levels fall below optimal range. Testing determines appropriate doses since requirements vary based on sun exposure, skin tone, and genetic factors.
Methylated B vitamins provide active forms that bypass genetic variants. B6 at 50-100 mg supports neurotransmitter synthesis as cofactor for multiple enzymes. B12 at 1000 mcg in methylcobalamin form supports methylation pathways. Methylfolate at 400-800 mcg works better than folic acid for those with MTHFR polymorphisms.
Magnesium glycinate at 300-400 mg daily improves sleep quality and reduces anxiety through GABA receptor modulation. This form absorbs better and causes fewer digestive side effects than other types. Deficiency appears common in depression with studies showing 65% of depressed patients have low magnesium levels.
Amino Acids and Methylation Support
SAMe (S-Adenosyl Methionine) at 400-1600 mg daily supports methylation and neurotransmitter production. Studies show effectiveness comparable to antidepressants with fewer side effects. Starting doses should begin low and increase gradually to avoid activation effects.
5-HTP at 50-200 mg daily converts to serotonin in the brain. Taking with B6 enhances conversion. This supplement works best for those with low serotonin rather than other neurotransmitter imbalances. L-Theanine at 200-400 mg daily increases GABA and reduces anxiety without sedation.
Herbal and Plant-Based Supplements
Curcumin at 500-1000 mg daily with black pepper reduces inflammation and increases BDNF production. Studies show antidepressant effects through multiple mechanisms including monoamine modulation and neurogenesis support.
Probiotics using multi-strain formulas with Lactobacillus and Bifidobacterium species at CFU counts of 10-50 billion support gut-brain axis function. Different strains produce different effects, making comprehensive formulas more effective than single-strain products.
Adaptogenic Herbs
Rhodiola rosea at 200-600 mg daily reduces fatigue and improves stress response as adaptogenic herb. Ashwagandha at 300-600 mg daily lowers cortisol and reduces anxiety. Holy basil at 300-600 mg daily supports HPA axis function and promotes resilience.
These supplements work best when combined with dietary and lifestyle interventions rather than used alone. Nutrient injections provide another delivery method for those with absorption issues.
What Advanced Treatments Does Functional Medicine Offer?

Functional medicine incorporates transcranial magnetic stimulation, neurofeedback, IV nutrient therapy, and ketamine treatment for treatment-resistant depression.
Brain Stimulation Therapies
Transcranial magnetic stimulation uses magnetic pulses to stimulate underactive brain regions involved in mood regulation. Sessions last 30-60 minutes, 5 days weekly for 4-6 weeks. FDA approval for major depression came after studies showed 50-60% response rates in treatment-resistant cases.
Neurofeedback trains patients to create healthier brain patterns through real-time monitoring. Improving alpha and theta wave balance reduces symptoms. Studies show sustained improvements lasting months after treatment completion.
Intravenous Nutrient Therapy
IV therapy delivers nutrients directly into bloodstream, bypassing digestive absorption. Common protocols include high-dose vitamin C at 15-25 grams, Myers cocktail with magnesium, calcium, B vitamins, and vitamin C, NAD+ for mitochondrial support, and glutathione for detoxification support.
Ketamine and Psychedelic Medicine
Ketamine therapy under medical supervision creates rapid antidepressant effects through NMDA receptor modulation. Studies show 70% response rates in treatment-resistant depression with effects appearing within hours rather than weeks.
Trauma Processing Techniques
EMDR uses bilateral stimulation to reprocess traumatic memories affecting mood. Originally developed for PTSD, research shows effectiveness for recurrent depression through addressing underlying trauma patterns.
Light and Environmental Therapy
Light therapy provides 10,000 lux full-spectrum light exposure for 30 minutes daily. Particularly effective for seasonal affective disorder, this treatment regulates circadian rhythms and melatonin production with minimal side effects.
How Long Does Functional Medicine Take to Improve Depression?
Most people notice initial improvements within 2-4 weeks, with significant symptom reduction by 3-6 months of consistent treatment.
Timeline varies based on depression severity, duration, root causes, compliance with recommendations, and medication use requiring gradual tapering under supervision.
Weeks 1-2 typically show energy improvements and increased sleep quality. Weeks 3-4 bring mood stabilization and improved mental clarity. Months 2-3 produce significant reduction in core depressive symptoms. Months 4-6 establish sustained improvements with new habits becoming automatic. Months 6-12 allow many to achieve remission or substantial recovery.
Some individuals respond rapidly to specific interventions like vitamin D correction or gut healing protocols. Others require longer treatment addressing multiple imbalances simultaneously.
Factors affecting timeline include severity with mild cases responding faster than severe cases, duration where recent onset improves quicker than chronic depression, root causes since nutrient deficiencies correct faster than gut dysbiosis, and compliance where consistent implementation produces better outcomes.
Can Functional Medicine Work with Conventional Treatment?
Functional medicine works alongside antidepressants and psychotherapy or serves as alternative approach depending on individual circumstances and severity.
Never discontinue medications without medical supervision. Stopping antidepressants abruptly causes withdrawal symptoms including nausea, irritability, insomnia, and mood changes. Some people gradually reduce doses under practitioner guidance as underlying causes resolve. Others maintain low doses while using functional medicine to minimize side effects.
Functional medicine integrates best with psychotherapy including CBT, DBT, or other modalities, conventional medical care from psychiatrists or primary care physicians, and support systems through family, friends, and community groups. The goal focuses on optimal outcomes using appropriate tools for each person.
Mental health treatment through integrative approaches combines the best of conventional and natural medicine. Research supports this combination producing better results than either approach alone in many cases.
Frequently Asked Questions
Is functional medicine covered by insurance for depression treatment?
Coverage varies significantly between insurance providers and plans. Some insurance companies reimburse functional medicine consultations when provided by licensed physicians or naturopathic doctors. Labs and supplements typically require out-of-pocket payment. Many patients find the investment worthwhile due to comprehensive care and long-term results.
How much does functional medicine treatment for depression cost?
Initial consultations range from $200-500 depending on practitioner experience and location. Comprehensive lab testing costs $500-2000 based on panels ordered. Monthly supplement expenses typically run $100-300. Follow-up visits cost $150-300 per session. Total investment for the first three months averages $2000-4000.
Can I stop taking antidepressants if I start functional medicine?
Never discontinue antidepressants without medical supervision from your prescribing physician. Functional medicine works effectively alongside medication initially. Some patients gradually taper medications under careful monitoring as root causes resolve and symptoms improve. Others continue low doses long-term while using functional approaches to enhance effectiveness and reduce side effects.
What types of testing does functional medicine use that regular doctors don't?
Functional medicine practitioners order comprehensive panels beyond standard screening. Micronutrient testing measures intracellular vitamin and mineral levels rather than just serum values. Comprehensive stool analysis examines beneficial bacteria, pathogenic organisms, digestive enzyme function, and inflammation markers. Organic acids testing reveals metabolic dysfunction, neurotransmitter metabolites, and mitochondrial health. Food sensitivity panels identify IgG reactions causing chronic inflammation.
How long before I see results with functional medicine for depression?
Initial improvements typically appear within 2-4 weeks of starting treatment. Energy levels often improve first, followed by sleep quality and mental clarity. Mood stabilization usually occurs around weeks 3-4 of consistent intervention. Significant symptom reduction becomes apparent at 3-6 months when addressing multiple root causes simultaneously. Some interventions like vitamin D correction or blood sugar stabilization produce faster results.
Final Thoughts
Functional medicine treats depression by addressing biological imbalances including gut dysbiosis, nutrient deficiencies, inflammation, hormonal disruption, and environmental factors. This approach provides personalized care based on comprehensive testing and root cause identification.
Research supports the effectiveness of dietary intervention, targeted supplementation, lifestyle modification, and advanced therapies for depression management. The gut-brain axis represents a particularly important target, with microbiome restoration showing significant therapeutic potential in recent studies.
Depression rates continue rising, particularly among young adults. Functional medicine offers evidence-based alternatives and complements to standard psychiatric care, addressing the whole person rather than isolated symptoms. Working with qualified practitioners allows for safe, effective integration of multiple therapeutic modalities.
The connection between physical and mental health cannot be separated. What affects the gut affects the brain. What affects hormones affects mood. What affects inflammation affects cognitive function. Treating the whole person through integrative approaches produces lasting results that symptom-focused treatment cannot achieve.
You May Also Like
.png)
.png)



%201.png)


.png)
.png)



.png)
.png)
.png)
.png)
.png)
.png)
.png)
.png)

.png)
.png)
.png)
.png)

.png)
.png)

.png)
.png)






.png)




.png)
.png)
.png)

.png)

.png)